Our Expertise
Our Expertise
The SPOR Evidence Alliance specializes in supporting knowledge synthesis, guidelines development, and knowledge translation in a purpose-driven, context-sensitive, and patient-oriented research environment. SPOR Evidence Alliance researchers work collaboratively with decision-makers and other stakeholders to produce health research that is fit-for-purpose, thus avoiding any research waste.
Knowledge Synthesis
A knowledge synthesis (also known as evidence synthesis) uses specific, rigorous and transparent methods to bring together information from multiple studies that have looked at the same topic to make sense of their findings. This allows health policy and practice decisions to be made based on all available scientific information, rather than a single study or expert opinion, which can be misleading.
Our approach is to integrate decision-makers throughout the research process to produce knowledge that is relevant and tailored for decision-maker needs.1
There are many different approaches to knowledge synthesis. You can use the tool What Review is Right For You? to help you decide which approach would be most useful in answering the research question posed by the decision-maker(s).
A typical knowledge synthesis approach includes the following 9-step process:
Click on each of the steps in the figure below for more information.
Research question is matched to an appropriate knowledge synthesis method in line with the purpose and objective of the research. A team to conduct the research is then set up including members with expertise in the knowledge synthesis method selected, clinical experts, knowledge users, and whenever possible, patients and research trainees/ graduate students. Research question is further refined and developed by clarifying the key elements (e.g., population(s), intervention(s), comparator(s) and outcomes) used to develop the research question. All outcomes that are of importance to our knowledge users are ranked and prioritized by patients and knowledge users using an online group ranking technique. Researchers and knowledge users work together to refine the question(s), as needed. A protocol for the planned knowledge synthesis is developed in consultation with all knowledge users and stakeholders. The protocol follows the reporting guideline, PRISMA-P2, and is peer-reviewed and registered with either PROSPERO or Open Science Framework. A summary of the registered protocol is also published under Our Projects. A work plan outlining the protocol, knowledge user engagement strategy, budget, and timeline is prepared. The work plan must be approved by the knowledge user before starting the review. Multiple electronic libraries (e.g., MEDLINE, EMBASE) including those with specialized clinical areas (e.g., PsycINFO for mental health) are searched. An experienced librarian develops the search terms, which are peer-reviewed by another librarian using the Peer-Review of Electronic Search Strategies (PRESS)3. Grey literature are also considered. A two-level screening process is used beginning with the screening of titles and abstracts of all records from the literature search. Potentially relevant full-texts articles are then screened for relevance. Each phase of screening begins with a pilot-test to make sure reviewers have sufficient agreement (>75%). Each title and abstract and full-text article is reviewed by two independent reviewers and any disagreements are resolved by discussion. Authors of primary studies are contacted when eligibility is unclear. A standardized form for data collection is developed and pilot-tested for agreement (>75%) between reviewers. Data from each article is collected by two independent reviewers. Disagreements between reviewers are resolved by discussion. If a study is missing important information, authors of primary studies are contacted. When applicable, each study is assessed for risk of bias using appropriate appraisal tool by two independent reviewers. This step also begins with a pilot-test to establish agreement between reviewers and any conflicts are resolved by discussion. Both qualitative and quantitative analyses are considered depending on the knowledge synthesis method and the types of evidence included. Appropriate reporting guidelines available on the EQUATOR Network website for the specific knowledge synthesis is used to prepare the final report. Manuscripts are published in a peer-reviewed journal. If the journal is not open-access, a pre-publication version of the manuscript is posted on Our Projects tab. A 1-page research brief is prepared to provide a high-level summary of the research findings.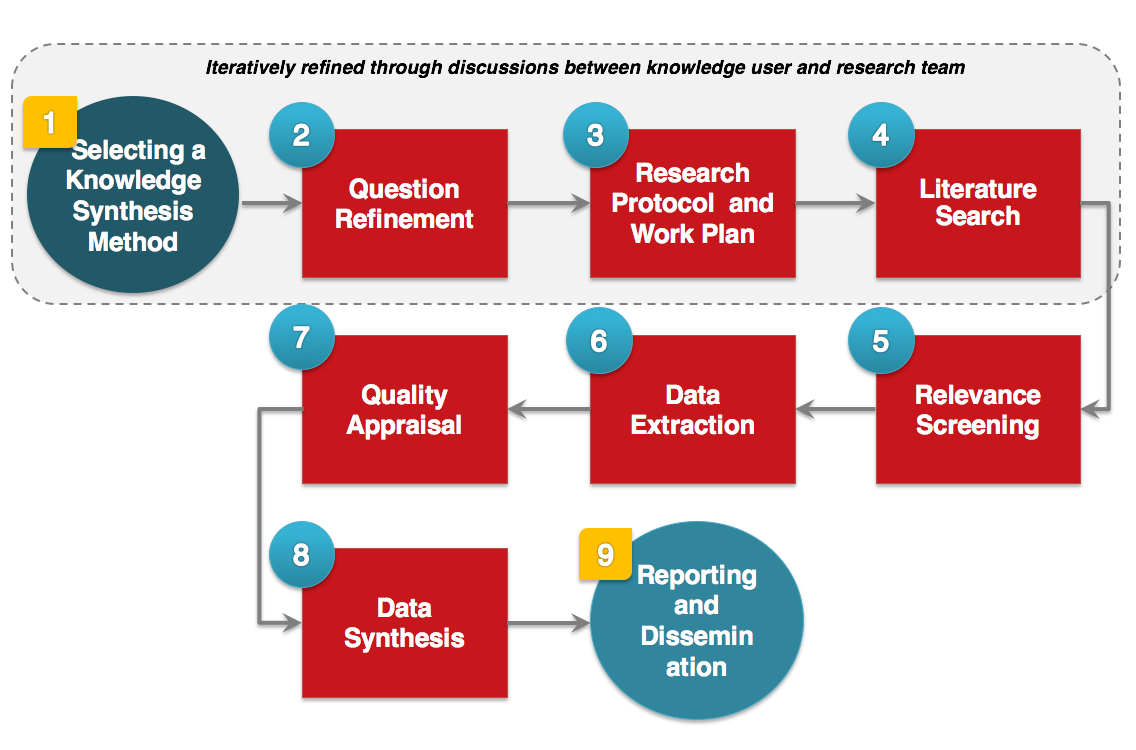
1. Selecting a Knowledge Synthesis Method
2. Question Refinement
3. Research Protocol and Work Plan
4. Literature Search
5. Relevance Screening
6. Data Extraction
7. Quality Appraisal
8. Data Synthesis
9. Reporting and Dissemination
Guidelines Development
A guideline is an evidence-based or consensus-based statement prepared to help improve the quality and consistency of practice for specific clinical or public health conditions or situations. They incorporate the most current information based on all available scientific evidence and professional opinions into a framework of best practices to promote the best patient and population outcomes.
Our goal is to support the development of more patient-centered and end-user-friendly guidelines using an integrated knowledge translation approach.
Guidelines are developed using a rigorous methodology and generally include the following 7-step process:
Click on each of the steps in the figure below for more information.
One a clinical practice guideline is approved using the SPOR Evidence Alliance priority setting process, a research team is set up. The primary research team consists of methods experts and experienced research staff in knowledge synthesis, guideline development and knowledge translation. Knowledge users are consulted to appoint an Expert Panel consisting of 10-15 multidisciplinary members, including patients (if possible) and healthcare providers. Chairs of the Expert Panel are nominated based on their objectiveness, responsiveness, and ability to facilitate group decisions. None of the research teams or Expert Panels can have any potential/perceived conflicts of interest. Training on disclosure of conflicts of interest, group participation, and expectations is provided to panel members. One a clinical practice guideline is approved using the SPOR Evidence Alliance priority setting process, a research team is set up. The primary research team consists of methods experts and experienced research staff in knowledge synthesis, guideline development and knowledge translation. Knowledge users are consulted to appoint an Expert Panel consisting of 10-15 multidisciplinary members, including patients (if possible) and healthcare providers. Chairs of the Expert Panel are nominated based on their objectiveness, responsiveness, and ability to facilitate group decisions. None of the research teams or Expert Panels can have any potential/perceived conflicts of interest. Training on disclosure of conflicts of interest, group participation, and expectations is provided to panel members. One a clinical practice guideline is approved using the SPOR Evidence Alliance priority setting process, a research team is set up. The primary research team consists of methods experts and experienced research staff in knowledge synthesis, guideline development and knowledge translation. Knowledge users are consulted to appoint an Expert Panel consisting of 10-15 multidisciplinary members, including patients (if possible) and healthcare providers. Chairs of the Expert Panel are nominated based on their objectiveness, responsiveness, and ability to facilitate group decisions. None of the research teams or Expert Panels can have any potential/perceived conflicts of interest. Training on disclosure of conflicts of interest, group participation, and expectations is provided to panel members. The research team prepares a clinical practice guideline protocol with details on the research questions, objectives, and methods. The Expert Panel reviews the protocol, and the revised version is sent for review by the knowledge users, any relevant Canadian guideline developers, patients, and stakeholders. The protocol is then sent for external peer-review and is revised accordingly. The final protocol is registered with a registry database, submitted for peer-reviewed publication, and then the published (or per-published) version is posted in Our Projects tab. The research team prepares a clinical practice guideline protocol with details on the research questions, objectives, and methods. The Expert Panel reviews the protocol, and the revised version is sent for review by the knowledge users, any relevant Canadian guideline developers, patients, and stakeholders. The protocol is then sent for external peer-review and is revised accordingly. The final protocol is registered with a registry database, submitted for peer-reviewed publication, and then the published (or per-published) version is posted in Our Projects tab. The Expert Panel prepares a draft of the guideline recommendations using the GRADE guidance and votes on the recommendations during a face-to-face meeting. The research team prepares the guideline report based on the recommendations. The recommendations are sent for external peer-review and submitted for publication in a peer-reviewed journal. The final publication is posted in Our Projects tab. The research team creates user-friendly resources to support dissemination and implementation of recommendations.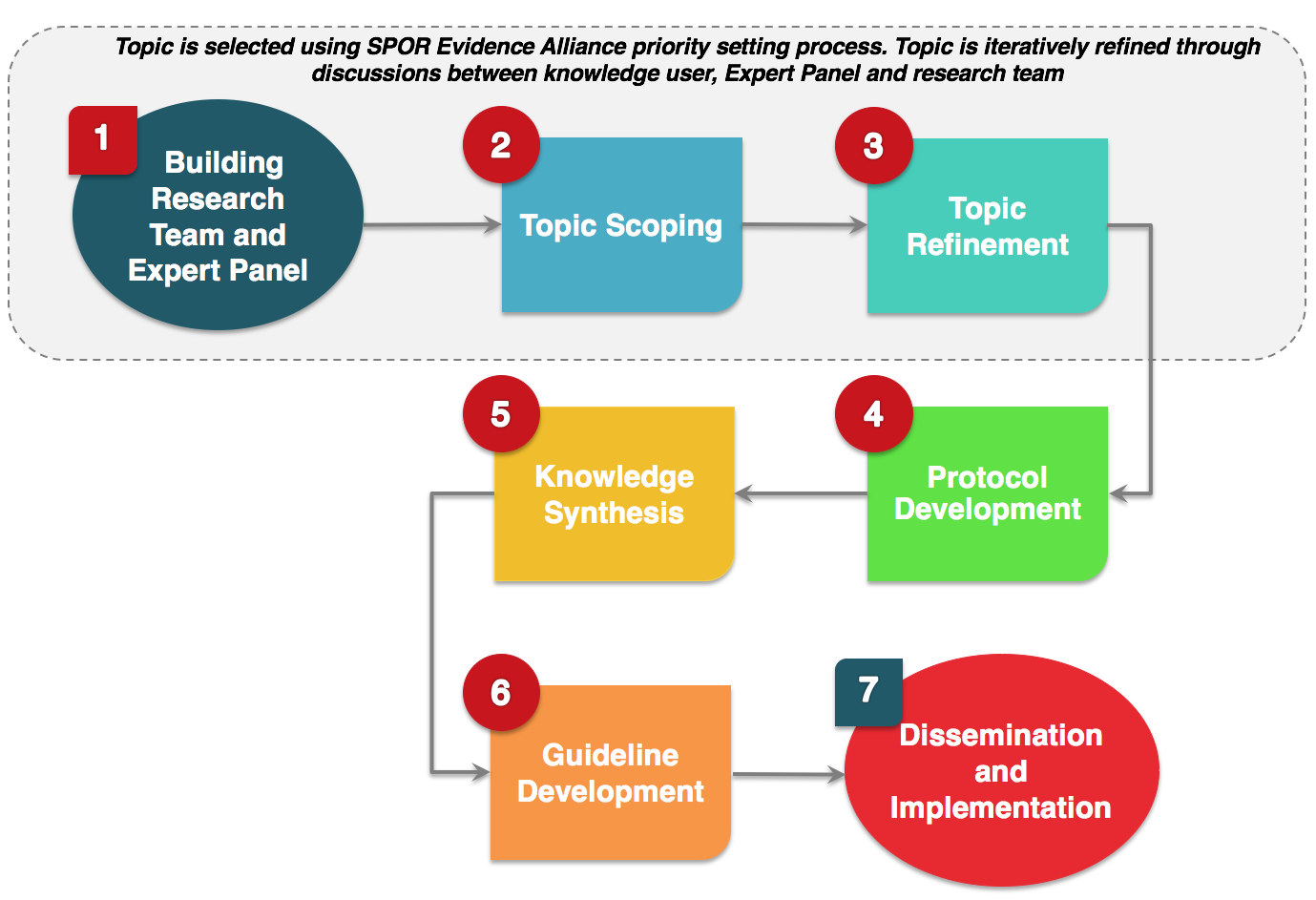
1. Building Research Team and Expert Panel
2. Topic Scoping
3. Topic Refinement
4. Protocol Development
5. Knowledge Synthesis
6. Guideline Development
7. Dissemination and implementation
Knowledge Translation
Knowledge translation is the process of summarizing, distributing, sharing, and applying the knowledge uncovered by researchers to improve the health of Canadians, and strengthen the health care system through the use of services and interventions proven to be more effective.
Our philosophy is to use theory and evidence to guide our knowledge translation approach. We publish all knowledge products (such as patient-friendly infographics, plain language summaries, research briefs, and brochures) on our website.
Implementation of guidelines
For all guidelines, an integrated knowledge translation approach is used. This involves engaging all decision-makers and stakeholders to identify the needs and preferences of the end-users by assessing the barriers and facilitators to uptake of the recommendations.
We also use current best evidence to design our strategy for guideline adoption. To identify evidence-informed knowledge translation strategies, we conduct grey literature searches using established databases.
References
- Gagnon ML. Moving knowledge to action through dissemination and exchange. Journal of clinical epidemiology. 2011;64(1):25-31.
- Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ (Clinical research ed). 2015;349:g7647-g7647.
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. Journal of Clinical Epidemiology. 2016;75:40-46.
